Current Good Manufacturing Practices
The FDA’s current Good Manufacturing Practices (cGMP) regulate proper manufacturing process and facility design, monitoring, and control of biopharmaceutical products to ensure the identification, strength, Quality, safety, and purity of drug products.
Establishing rigorous operating procedures, acquiring acceptable Quality raw materials, identifying and looking into product Quality variations, and maintaining trustworthy testing labs are all part of this. If properly implemented, this formal system of controls at a pharmaceutical company aids in preventing instances of contamination, confusion, divergence, failure, and error. This guarantees that pharmaceutical items adhere to their Quality criteria.
The cGMP criteria were created with flexibility in mind, allowing each producer to choose how to best implement the required controls by utilizing design, processing, and testing techniques that are based on good scientific principles. Due to the regulations’ flexibility, businesses can employ cutting-edge methods and technology to continuously improve Quality.
The “c” in cGMP is often also considered to stand for “contemporary,” because it is forcing businesses to adopt modern processes and technology to abide by the rules. To avoid contamination, confusion, and errors, systems and equipment that may have been top-of-the-line 10 or 20 years ago, may now be deemed less than acceptable. It is crucial to remember that the cGMP are only necessary minimums. Many pharmaceutical factories have already adopted thorough, contemporary Quality systems and risk management strategies that go above and beyond these minimum requirements.
History
In 1968, the first WHO draft text on GMP was approved. The WHO GMP was quickly acknowledged as a crucial component of the WHO Certification Scheme in 1969, when the World Health Assembly proposed the first iteration of the scheme to assess the Quality of pharmaceutical products being sold on the international market. In 1991, the Expert Committee on Biological Standardization (ECBS) then adopted a supplementary annex on biological medicinal products that establishes the general methodology for the Quality control of biological medicines, which include items like vaccines, blood and blood products, antigens, cell and tissue therapies, biopharmaceutical products, and others.
Today, more than 100 nations have successfully incorporated the WHO GMP requirements into their national drug legislation, and numerous other nations have done the same while creating their own GMP standards. The WHO Certification Scheme and prequalification of vaccines for procurement by UN agencies both continue to be based on the WHO GMP.
Importance
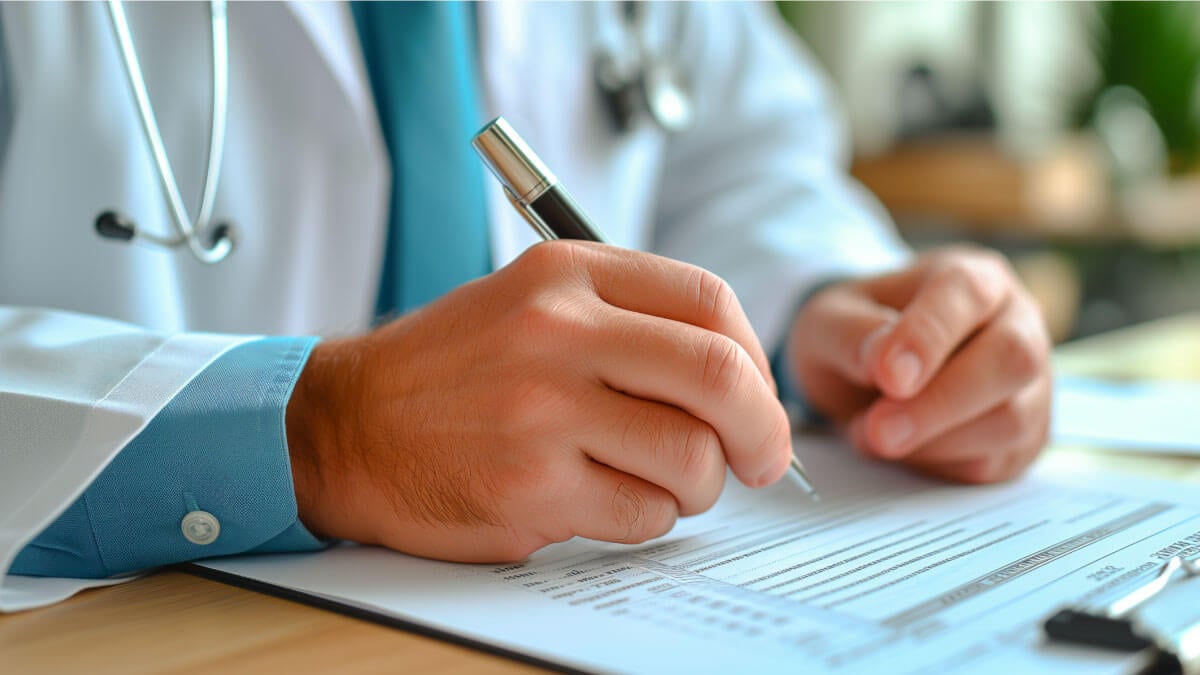
Typically, a consumer cannot tell whether a drug product is safe or effective by scent, touch, or sight. Testing is required under cGMP; but testing alone is not sufficient to guarantee Quality. Most of the time, only a small portion of a batch is tested.
A medicine maker might examine 100 of a batch of 2 million tablets, for instance, allowing the majority of the lot to be used by patients rather than being wasted on testing. To ensure that Quality is embedded into the design and manufacturing process at every stage, medications must be made under the circumstances and methods mandated by the cGMP rules. A few examples of how cGMP regulations serve to ensure the safety and efficacy of drug products include facilities that are in good condition, equipment that is properly maintained and calibrated, workers who are qualified and thoroughly trained, and processes that are dependable and reproducible.
The FDA inspects pharmaceutical production facilities throughout the world, including those that create both active ingredients and finished goods. Inspections are carried out by highly skilled FDA personnel using a uniform procedure. FDA also relies on industry and consumer reports of potentially problematic drug items. These reports are frequently used by FDA to determine which facilities require inspections or investigations. The majority of businesses that are examined are discovered to be compliant with cGMP guidelines.
cGMP Objectives
- To ensure the items are consistently produced and held to the required standards of Quality.
- Occupied with every facet of production and Quality assurance.
- General supervision and control throughout the production of cosmetics.
If the product’s Quality is dependent on the raw materials, production, Quality control procedures, building, equipment, and employees involved, make sure the client receives the product of the stipulated Quality.
cGMP in the Pharma Industry
Consumers have no means of knowing whether the substance they are ingesting is safe and effective. Testing alone cannot guarantee Quality. Medications must be manufactured in compliance with the conditions and procedures required by the cGMP rules to guarantee that Quality is incorporated into the design and manufacturing process at every level. Maintaining facilities, equipment that is correctly calibrated, personnel who are qualified and trained, and processes that are dependable and repeatable are just a few examples of such conditions and practices.
The cGMP guidelines include the following aspects to take into account:
- Keep manufacturing facilities sanitary and clean.
- Guarantee a regulated environment in place to avoid cross-contamination that could make the product unfit for human consumption.
- Manufacturing procedures must be precisely controlled and defined. Every essential procedure is frequently validated to guarantee consistency and adherence to the requirements.
- Any modification that could impact the efficacy of the medicine is approved. adhering to best documentation practices.
- Operators receive regular training on document procedures. maintaining records—manually or digitally—during the manufacturing
- Any discovered deviations must be looked into and recorded.
- Records of production and distribution are required so that a batch’s whole history may be tracked, stored, and retrieved.
- Products’ quality must not be put at unnecessary risk during distribution.
- Any batch must be recalled from sale or supply; hence, a recall system must be in place.
- The reasons for Quality flaws must be looked into, complaints about marketed products must be examined, and suitable steps must be made to address the defective items and avoid their recurrence.
cGMP Violations
A company may recall a product if the failure to comply with cGMP results in the distribution of a drug that, for example, contains too little active ingredient and does not provide the benefit claimed on the label. Taking these medications off the market safeguards the general public from additional harm. Although the FDA cannot compel a manufacturer to recall a medicine, most do so voluntarily or at the FDA’s request. The FDA has the authority to issue a public alert and can confiscate a medicine if a manufacturer refuses to recall it.
Even in cases when there is no clear evidence that an error is impairing a drug’s effectiveness, the FDA is nonetheless permitted to file a seizure or injunction case in court to resolve cGMP violations. When the FDA does file a seizure action, the agency requests a court order allowing federal agents to seize the adulterated pharmaceuticals. At this time, the FDA also requests the court to order a corporation to stop breaking cGMP. Court orders requiring businesses to take numerous actions to address cGMP violations are frequently issued in both seizure and injunction cases. These actions might include fixing facilities and equipment, enhancing sanitation and cleanliness, carrying out additional tests to confirm Quality, and improving employee training. Due to cGMP violations, the FDA may even file criminal charges and impose fines.
Conclusion
By enforcing cGMP, the FDA ensures that pharmaceuticals are safe for end users and that their health benefits outweigh their dangers. As demonstrated in 2012 when faulty compounding at the New England Compounding Pharmacy sparked an outbreak of fungal meningitis that resulted in 64 deaths, 751 injuries, and 25 counts of second-degree murder, properly implemented cGMP should not be seen as a regulatory burden but rather as a reliable safeguard against potentially disastrous outcomes.
Simply said, a business must have the following to adhere to cGMP: correctly calibrated and maintained equipment; qualified, well-trained employees, as well as dependable, repeatable operating procedures.
If subpar supplies arrive at your manufacturing site, your company is clearly lacking reliable systems. Upstream control implementation is no longer possible. Therefore, working knowledge of your supplier’s controls and Quality management system is essential for you as a pharmaceutical company to have “strong systems.” It also needs a strong alliance and trust.
Additional resources

How to Implement the Continuous Improvement Cycle | Scilife
Even an organization with stellar leadership and a solid core of employees experiences hiccups from time to time. Despite having assembled all the ...
How to assess and enhance your Quality Management Maturity | Scilife
As the life sciences industry becomes increasingly regulated and competitive, quality management has become more vital than ever. Are you confident ...
Best Quality Management Software (QMS) for Life Sciences | Scilife
The right electronic Quality Management System (eQMS) can help strengthen your compliance processes and build a culture of quality within your ...
How to write a good quality plan for medical devices | Scilife
In life sciences, especially if you’re in the medical device industry it becomes harder to manage projects in accordance with your company’s quality ...
Turn quality into your brightest asset with Scilife
