GCP: Good Clinical Practice
GCP is the abbreviation of Good Clinical Practices.
GCP is an international quality standard that lays down by a guideline named ICH E6 (R2) Good clinical practice. ICH is an international body that defines standards that governments can transpose into regulations for clinical trials involving human subjects. This guideline ensures the experimentation on humans is done for the sake of advancement in medical sciences and serves as a quality benchmark as well as a moderator that keeps such experimentation in check. It also outlines the requirements of a clinical trial and the roles and responsibilities of the officials involved in it.
The current ICH guideline defines the GCP term as a standard for the design, conduct, performance, monitoring, auditing, recording, analyzing, and reporting of clinical trials that gives assurance that the knowledge and reported results are credible and accurate, and that the rights, integrity, and confidentiality of trial subjects are protected. WHO also published a handbook GCP Guidance for implementation which is named “Handbook for good clinical research practice (GCP)”. This guideline consists of 14 Principles, which are as follows:
WHO Principles of GCP
- Principle 1: Research that involves humans should be scientifically sound and conducted in line with basic ethical principles originating from the Declaration of Helsinki. Three principles of equal importance associated with basic ethics, particularly recognized for persons, beneficence, and justice, permeate all other GCP principles.
- Principle 2: Research that involves humans should be described clearly in a written detailed protocol, and scientifically justified.
- Principle 3: Before the research that involves humans is begun, possible risks, obstacles, discomforts, and expected benefit(s) for the individual research subject and society should be determined.
- Principle 4: Research that involves humans should be started on the condition that the expected benefit(s) for the individual research subject and society clearly outweigh the risks.
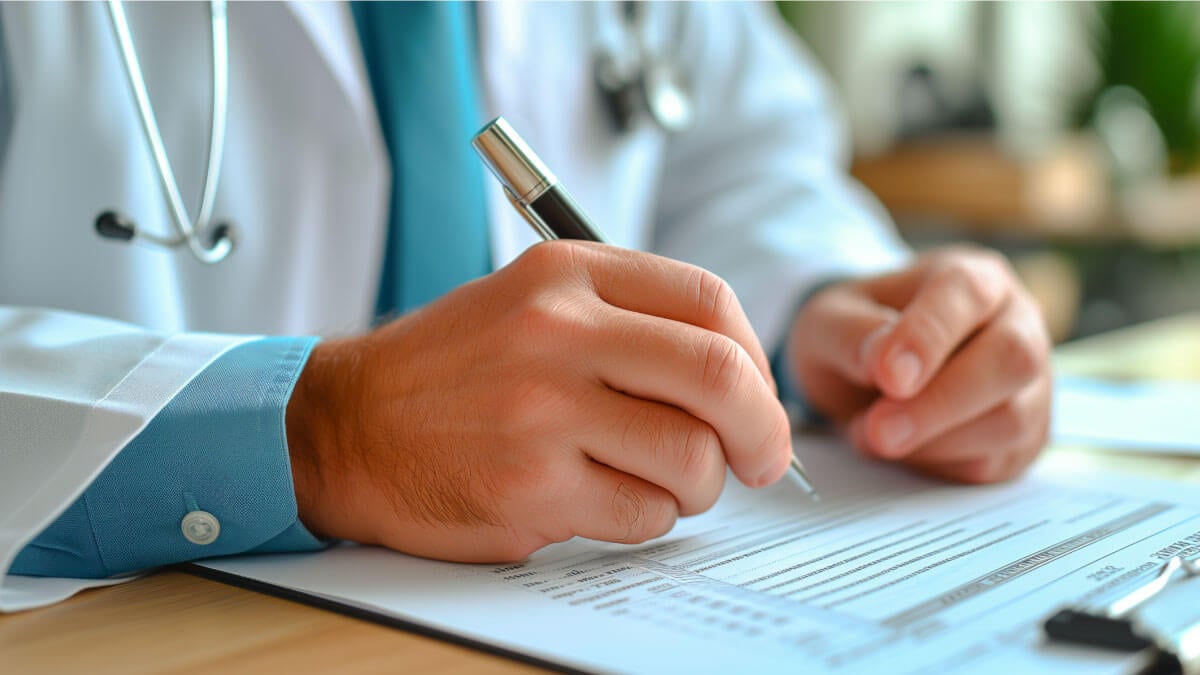
- Principle 5:Research that involves humans should get approval/favorable opinion from the independent ethics committee/institutional review board (IEC/IRB) prior to initiation.
- Principle 6:Research that involves humans should be performed in compliance with the approved protocol.
- Principle 7:Freely given informed consent should be collected from each individual research subject prior to research participation in accordance with national culture(s) and requirements.
- Principle 8: Research that involves humans should be maintained only if the benefit-risk profile of the involved humans remains favorable.
- Principle 9: Qualified and duly licensed medical personnel should be responsible for the medical care of individual research subjects, and for any medical decision(s) made on their behalf.
- Principle 10: All individuals that are involved in a trial should be qualified by education, training, and experience to perform their respective task(s) and currently licensed to do so, where required.
- Principle 11: All clinical trial information should be documented, handled, and stored in a way that allows accurate reporting, interpretation, and verification.
- Principle 12: The confidentiality of information that could identify subjects should be secured, respecting the privacy and confidentiality rules in accordance with the applicable regulatory requirement(s).
- Principle 13: Investigational products should be manufactured, handled, and stored according to the applicable Good Manufacturing Practice (GMP) and should be used in accordance with the approved protocol.
- Principle 14: Systems with procedures that ensure the quality of every feature of the trial should be implemented.
Additional resources

How to Implement the Continuous Improvement Cycle | Scilife
Even an organization with stellar leadership and a solid core of employees experiences hiccups from time to time. Despite having assembled all the ...
How to assess and enhance your Quality Management Maturity | Scilife
As the life sciences industry becomes increasingly regulated and competitive, quality management has become more vital than ever. Are you confident ...
Best Quality Management Software (QMS) for Life Sciences | Scilife
The right electronic Quality Management System (eQMS) can help strengthen your compliance processes and build a culture of quality within your ...
How to write a good quality plan for medical devices | Scilife
In life sciences, especially if you’re in the medical device industry it becomes harder to manage projects in accordance with your company’s quality ...
Turn quality into your brightest asset with Scilife
